Abstract

Introduction:
Life expectancy after allogeneic stem cell transplant (HCT) in pediatric HCT recipients remains lower than expected compared to the age and sex matched population. In adults late fatal infections (LFI) contribute to 10-20% of all death, however very little data exists regarding deaths in pediatric patient (pts) from infections occurring 2 years or later after HCT. In order to address this, we performed an analysis of late fatal infections (LFI) in pediatric HCT recipients using Center for International Blood and Marrow Transplant Research (CIBMTR) database.
Methods:
Pts who received first HCT between 01/1995 and 12/2011, reported to the CIBMTR who survived disease-free at 2 years or longer following HCT were included in the analysis. Pts transplanted at centers with follow up completeness index < 80% at 4 years post HCT were excluded. Late fatal infections were described and their cumulative incidence was calculated as death from infectious complications occurring at least 2 years after HCT in eligible subjects. Risk factors for LFI were identified using Cox regression models. Pts with late relapse or second HCT (after 2 years) were censored at the event.
Results:
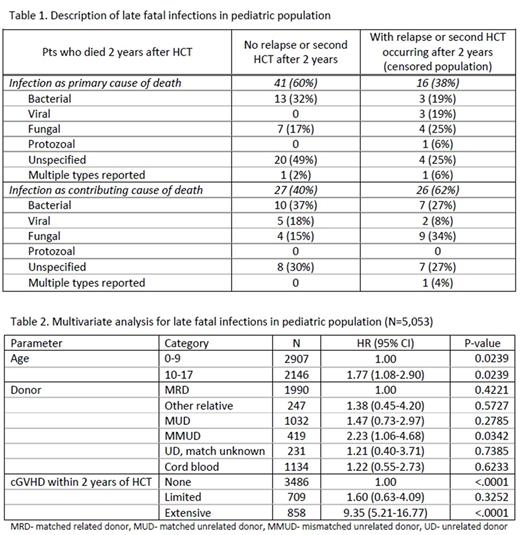
Outcomes of 5088 pts from 202 centers were analyzed. The median age at transplant was 9 (<1-18) years. 4064 (80%) and 977 (19%) pts received myeloablative and reduced intensity/non-myeloablative conditioning, respectively. Bone marrow, peripheral blood and cord blood were used as graft source in 3395 (67%), 553 (11%) and 1140 (22%) pts respectively. Invasive fungal infections prior to HCT was reported in 418 (8%) pts and 75 pts (1%) were HIV positive. Acute GVHD (aGVHD), limited or extensive cGVHD within 2 years of HCT occurred in 1522 (30%), 709 (14%) and 858 (17%) pts, respectively. There were 377 pts (7%) who died after 2 years from any cause. Infection, as a primary or contributing cause of death, was reported in 110 (2%) subjects and overall LFI contributed to 29% of all late deaths. Bacterial infections were most commonly reported LFI (Table1). The cumulative incidence of LFI in patients did not significantly increase with time after HCT, at 3, 5, 8, 10 and 12 years was estimated at 0%, 1%, 1%, 1% and 2% respectively.
In multivariate analysis, increasing age ≥10 years, receipt of MMUD and history of extensive cGVHD were associated with increased risk of LFI (Table 2). Diagnosis, history of aGVHD, recipient sex or use total body radiation based conditioning were not associated with risk of LFI.
Conclusions:
This is the first comprehensive analysis of LFI in large cohort of pediatric pts. Despite overall low late mortality, LFI in pediatric HCT recipients contributed to a significant proportion of all deaths occurring at least 2 years after HCT. Age, HLA match and history of extensive cGVHD were associated with increased risk of LFI. Risks of LFI do not diminish over 12 years of follow up.
Norkin: Celgene: Honoraria, Research Funding. Flowers: Pharmacyclics: Consultancy. Savani: Jazz Pharmaceuticals: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal